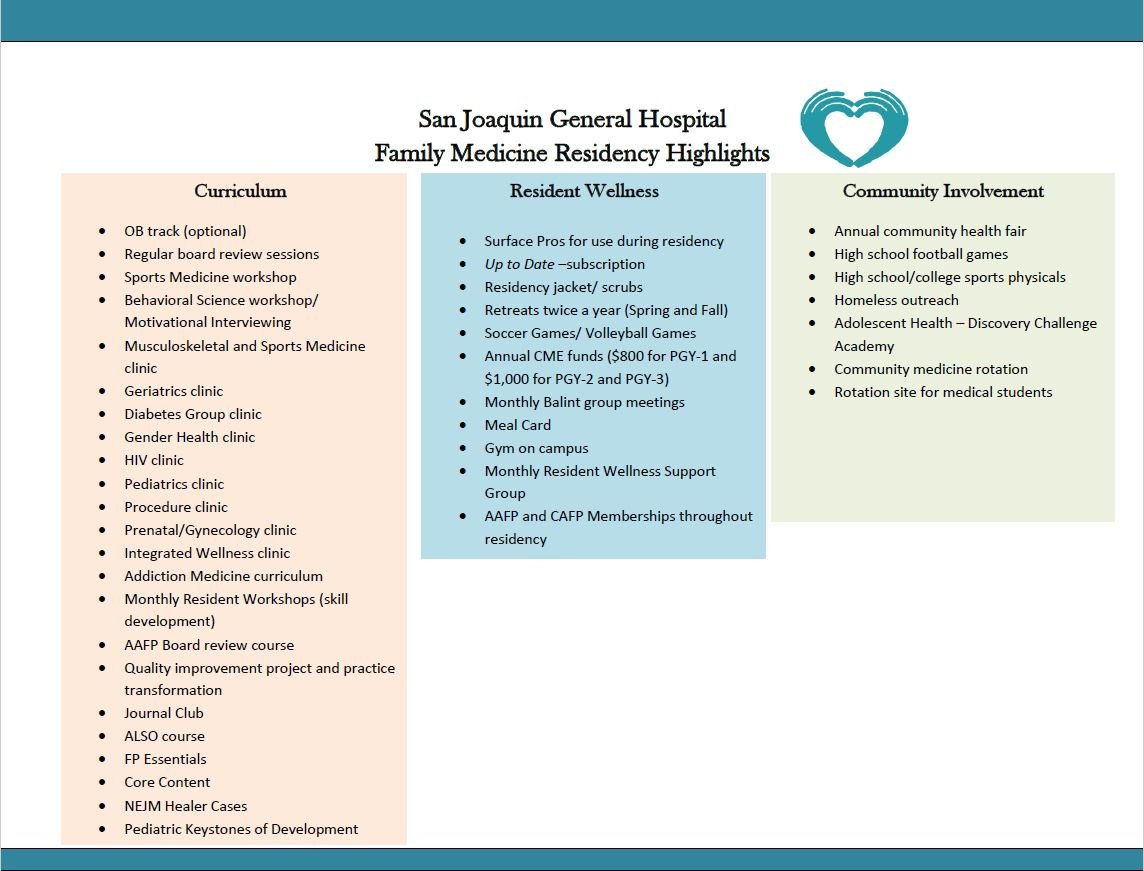
Our Curriculum
Please note, unless otherwise specified, the rotations blocks are each 4 weeks.
The San Joaquin General Hospital's Family Medicine Residency Program is structured to train thoughtful and caring physicians to be prepared for a diverse scope of practice in the field of family medicine. Our patient population is the underserved in San Joaquin County. Our residents see a broad range of pathology. The principal strength of San Joaquin General's program is the autonomy afforded to our residents in both the outpatient and inpatient services. On the outpatient services, residents rotate through our FQHC qualified clinics including our own family medicine clinic, sports medicine clinic, procedures clinic, geriatrics clinic, pediatric clinics, gender health clinic, sexual health clinic, and psychiatry clinic. On inpatient rotations, residents are responsible for acute care of all ages and at all stages of life including the intensive care nursery, labor and delivery, ICU, and the family medicine inpatient service.
Experience gained from direct patient care in both outpatient and inpatient settings are complemented by Wednesday afternoon didactics which range from case-based interactive discussions, to formal resident and faculty presentations, Jeopardy.
Below, you will find more detailed information about each of our rotations. Our residents typically rotate through two to four week blocks, for a total of 13 rotations each academic year. In the beginning of residency, there is a larger focus on inpatient medicine. Toward the end of residency (PGY-II and III), our residents spend the majority of their time in our outpatient clinics. Throughout all three years, residents rotate through several two week blocks of night float which covers our inpatient service and admissions from approximately 6pm to 6am (more details on night float at the bottom of the page).
Call Schedule (longitudinal)
Residents take "call" providing cross-coverage to our inpatient teams and admitting, on a varying basis depending on their current rotation and their current post graduate year. Our call shifts are 17 hour shifts including a half day of clinic followed by covering the inpatient service and admissions through the night. The call shifts are on average 1 – 2 times per month when on outpatient rotations. When our residents are on the inpatient adult, labor & delivery service, or inpatient pediatric service, call is every 6th day.
Inpatient Adult Family Medicine (multiple 2 or 4-week blocks)
The Family Medicine Inpatient Service at SJGH provides care to acute adults who are hospitalized. Patients are admitted from our clinic and the SJGH Emergency Department. Our inpatient service is staffed by a family medicine attending physician (rotating on a weekly basis), one to two senior residents (R3 and/or R2), and one to two interns. Clinical pharmacist, pharmacy students, medical students, and members of the billing/coding team also round with the service. Our inpatient teams care for patients with a high level of complexity (as expected in a safety net hospital) which includes sepsis, congestive heart failure exacerbation, acute gastrointestinal bleeds, as well as complications of chronic diseases, such as diabetes, hypertension, and cancer. We share a collaborative atmosphere with both the surgical and internal medicine residency programs at our community hospital who help to co-manage complex patients. When our patients need more intensive care, our patients are transferred to our ICU where their care is coordinated by the internal medicine team and the family medicine resident rotating through the ICU. Our ICU operates on a "closed" system which means when a patient is sent to the ICU, we no longer follow them until they are downgraded from the ICU. Under the guidance of the attending and senior residents, various inpatient procedures are performed on service, including thoracentesis, paracentesis, lumbar punctures, central line placements, and biopsies.
There are three 4-week inpatient adult family medicine blocks during intern year, two during second year, and one 4-week and one 2-week block in the subsequent years of training.
Inpatient Pediatric Medicine (multiple 4-week blocks)
The strength of our pediatric experience can be attributed to longitudinal teaching from both our pediatrics attendings and from the family medicine attendings. The inpatient service at SJGH provides acute inpatient care to pediatric population >14 years of age. We also have 4 weeks of newborn nursery at SJGH. The remainder of our pediatric inpatient rotations are at St. Joseph’s Hospital in Stockton. Our inpatient pediatric teams care for patients with a broad range of complexity, ranging from phototherapy for hyperbilirubinemia to managing complications in patients with cerebral palsy and sepsis. Our residents become skilled and confident in managing common bread and butter pediatric disease such as dehydration, asthma, RSV bronchiolitis, and neonatal fever. Invasive procedures typically include lumbar puncture to work up septic neonates. In addition to training received in the hospital, our residents also spend time with child protective services to learn more about how they can help our young patients.
There is one newborn medicine block during intern year and one inpatient pediatric block in the subsequent years of training.
Family Medicine Clinic (longitudinal + multiple 4-week blocks)
All residents are given a patient panel, where they care for their own personal population over the course of their three years at San Joaquin General. In addition to our own continuity clinics, residents also participate in longitudinal ambulatory experiences in behavior science and psychiatry. The responsibilities for our residents increases with their seniority. During the intern year, residents have only half a day each week for their continuity patients in the family medicine clinic. This increases to one full day a week for second years and third years (except when on the family medicine inpatient service). The census during the continuity clinic also progressively increases with seniority as well, with new interns initially seeing 4-5 patients in half-a-day, to 8-15 for the more senior residents. Preceptors from both the community and core faculty actively teach our residents during their clinic to utilize evidenced based medicine.
Continuity clinic is usually at least once a week, with clinic time increasing with seniority. Our residency program is more inpatient medicine focused at the start of residency (PGY-I), and more outpatient focused toward the end of the residency program (PGY-III).
Obstetrics (two, 4 week-blocks)
All interns will gain experience in obstetrics through two 4-week blocks in our unopposed labor and delivery floor. We are the only high-risk delivery labor and delivery unit in our county, providing us a great deal of complexity and experience usually only seen in tertiary centers. In addition to training on the labor and delivery service, we also spend two full days with other family medicine residents in the UC Davis network to train in the family medicine ALSO (advanced life support in obstetrics) course. Our residents easily make the requirements for the number of both vaginal and Cesarean deliveries at our hospital under the guidance of our obstetrics-fellowship trained family medicine attending and the supportive obstetricians & midwives. Our residents serve as first-assist for Cesarean sections as the obstetrics and gynecology service does not have residents. At the end of the two blocks, our residents not only gain experience regarding the bread and butter of obstetrics, but also gain exposure to high risk patients, multiple-gestation deliveries, Obstetric ultrasound, operative vaginal delivery, and perineal repair. After two blocks of obstetrics and the ALSO course, our residents can then begin taking care of continuity prenatal patients. These prenatal patients give the residents the opportunity to care for the mother prior to pregnancy, during delivery, and after delivery along with the newborn.
There are two blocks of obstetrics during the intern year, each lasting 4 weeks. After completion of the two obstetrics blocks, the resident becomes eligible to take care of their own continuity prenatal patient, for which the resident will be responsible for prenatal, perinatal, and postnatal care for the mother.
Musculoskeletal (multiple 2 or 4 week blocks)
Under the guidance of our attendings, we learn to develop clinical skills to prevent and manage sports-related injuries, as well as common musculoskeletal injuries in our family medicine patients. We rotate through sports medicine clinic with our sports medicine trained attending, focusing specifically on our musculoskeletal exam for diagnosis, and procedural training including joint injections. During this rotation, we also spend time with our orthopedic surgeons in their clinic and in the operating room as a first assist. In addition, we spend time in the casting room learning how to apply casts. Our residency program is responsible for providing sports medicine coverage for Stagg High School's football team. On Fridays, during football season, we are on the sidelines to intervene when there are any sports-related injuries. We also help our local community college and high school with sports physicals. The program also provides sports physicals at Discovery academy, an alternative high school operated by the California National Guard for high-risk youths.
This rotation lasts for 4 weeks in the intern year and can be taken as elective credit in further years.
Behavioral Science and Psychiatry (longitudinal)
During outpatient rotation residents frequently participate in dedicated psychology and psychiatry clinics, seeing patients along with an attending psychologist and psychiatrist. First-year residents are taught the basics of clinical diagnostic interviewing as well as evidence-based treatment for mild-to-moderate psychiatric disorders. Second- and third-year residents rotate more frequently with the attending psychiatrist and learn comprehensive psychopharmacology care for the more complicated patients. In addition, learning is facilitated through a seminar-based psychology workshop, where residents can get help with challenging cases and learn treatment techniques and interviewing skills. An emphasis is placed on teaching motivational interviewing to help the resident to have effective tools in motivating the ambivalent patient to positive behavior change, be it for a mental or substance use-related condition or for a medical condition such as chronic pain self-care.
Our mental health education spans the entire length of our residency, usually with several days out of the week dedicated to psychology and psychiatry clinic during our outpatient rotations.
Gynecology (single 4-week block)
In addition to our own gynecology clinic in our family medicine clinic, we spend a month with gynecologists in their outpatient and procedure clinic. We learn the all aspects of care for women including a family-oriented approach to common women's health issues. We learn about the common clinical problems in the ambulatory setting. In addition, we learn to perform pelvic exams and procedures with proficiency and skill, including IUD insertion and removal, Nexplanon insertion and removal, pap smears, and colposcopies. The focus of this rotation is to develop competence in the Well Woman Exam which includes performing appropriate breast and pelvic exam, identifying normal and abnormal exams and appropriate evaluation for abnormal exams.
This rotation lasts for 4 weeks and is only part of the PGY-III rotation schedule.
Intensive Care Unit (one 2-week blocks)
During the PGY-II years, our residents work alongside San Joaquin internal medicine residents in the adult intensive care unit to care for critically ill patients. Our ICU is a closed system (patients who enter the ICU have their care taken over by a designated ICU team). During this rotation, invasive procedures are practiced and refined including: arterial line placement, central venous catheter placement, lumbar puncture, thoracentesis, and paracentesis. Our residents also spend time learning how to use the ultrasound to help with fluid management, procedures, and detection of DVTs. In addition, our residents gain valuable experience with family discussions under the supervision of the ICU attendings.
Geriatric Medicine (longitudinal)
Under the guidance of our geriatric medicine fellowship trained family medicine attending, our residents spend a majority of their time in clinic, learning about the geriatric assessment, learning to maintain older adults in the community at the most independent level as possible through an interdisciplinary family medicine approach. We also gain exposure to long-term care including skilled nursing facilities, and rehabilitation centers. In clinic, we also work closely with our pharmacists, neurologists and psychiatrists in the diagnosis and treatment of dementia, and psychiatric disorders in the elderly. We spend time with a local hospice to learn about hospice care at facilities and at a patient's home.
We currently rotate through these sites:
Adult Protective Services
Hospice of San Joaquin
Geriatric Home Visits
Cardiology (single 4-week block)
This four-week rotation provides our residents a cardiology experience in the inpatient and outpatient setting. For most of the rotation, our residents work one-on-one with the attending cardiologist at our hospital. Our residents serve on the inpatient consult service and are the first contact for patients with a variety of cardiovascular diseases including acute coronary syndrome, acute decompensated heart failure, and arrhythmias. In the inpatient setting, residents are taught how to evaluate ejection fraction, how to read EKGs, and how to utilize the best pharmacotherapy for our patients. In the outpatient setting, residents participate in management of chronic conditions in the cardiology clinic, congestive heart failure clinic, and in the pulmonary hypertension clinic. Our residents participate in cardiac procedures including stress testing, electrical cardioversion, and even temporary transvenous pacemaker placement.
Community Medicine (longitudinal)
We care for those in our community and this rotation serves as a way for our residents to learn about how communities affect patients. Residents learn to engage with their communities by giving presentations and educating the community about primary and secondary prevention. Residents also visit community agencies such as our community lead screening program and Child Protective Services. Residents also work in our outreach clinic with our unhoused population, taking healthcare directly to our patient population. This rotation sheds light on the importance of the social determinants of health.
Emergency Medicine (2-week block and 4-week block)
Residents rotate through the emergency department during their first year for 2 weeks, and second and year for 4 weeks. Our emergency department is the only level III trauma center in our county. Our residents are supervised by attending physicians in the department of emergency medicine. As the only trauma center in our county, our residents are exposed to a wide variety of cases. Our residents also are able to perform many procedures while on their emergency medicine rotation including: central venous catheter placement, paracentesis, lumbar puncture, and laceration repair. This rotation helps our residents develop their clinical knowledge in the diagnosis and treatment of emergent medical conditions.
Procedure Clinic (multiple 2 or 4-week blocks)
Our procedure clinic is staffed by our faculty and you will have one on one teaching. Patients get referred from residency clinic as well as primary care offices part of our system and the outside community. We perform a wide variety of procedures typically performed in the outpatient setting, as listed here
Our procedure clinic is scheduled for our PGY-II and III residents.
Newborn nursery (4-week block)
During this 4-week block, residents work with pediatricians in the newborn nursery learning the general newborn physical examination. Residents gain experience in learning about screening tests and what to do with abnormal findings in newborns as well as manage hyperbilirubinemia, neonatal hypoglycemia, and neonatal abstinence syndrom.
Surgery (4-week block)
Training is provided by the general surgery department with emphasis on diagnosis, management, and timely referral for surgical evaluation. Residents are under the supervision of the Department of Surgery and they work alongside the surgical residents. Duties include both the inpatient surgical service and the outpatient surgical clinic. Residents are able to achieve competency in the diagnosis and management of a wide variety of surgical problems encountered by family physicians. Operating room experience is encouraged but not required. In addition, our residents are involved in the trauma activation team during their 4-week block, affording them direct experience in trauma care.
Night Float (multiple 2-week blocks)
Our program uses a "night float" system to cover our inpatient services during the evening and early morning hours. These night float rotations last for two weeks and involve admitting and cross-coverage for inpatient adult, inpatient pediatric, intensive care nursery, and the labor & delivery services. The night float team typically consists of a senior resident and a junior resident who work as a pair. The on-call attending is always available to back up our residents. The night float rotation allows for our residents to strengthen their self-sufficiency and their ability to triage across a broad range of services. Modernized on-call rooms are present for the residents during this rotation.
There are three 2-week-night float blocks in the first year, three night float blocks in the second year, and two night float blocks in the last year of residency. Night float is typically from 6pm to 6am, from Saturday to Thursday.
Electives (multiple 2 or 4-week blocks)
We offer our residents opportunities for elective rotations in their PGY-II and PGY-III years. Four week blocks are available for our residents to custom-tailor their educational experience to their future practice. Residents can choose from many of our home electives or the vast amount of electives within the UC Davis Medical Center system. Unfortunately, international electives are not available at this time. Off-site rotations are available if the resident is able to arrange their own malpractice insurance for the elective.